For months, different information has been floating around the news cycle about the novel coronavirus COVID-19. With students returning to Colorado Mesa University (CMU), there is a greater need than ever to get the facts straight. Here are a few myths busted about coronavirus.
Myth: The coronavirus is just like the flu.
COVID-19 and influenza do have similar symptoms such as a fever, cough and runny nose. They are also both transmitted through droplets in the air such as a sneeze, and can both be potentially severe or fatal.
However, COVID-19 has a litany of other symptoms that are still being figured out, and there is no vaccine available like there is with strains of influenza. According to the John Hopkins University of Medicine, COVID-19 also can have serious effects on the lungs, heart, kidneys and brain in ways that are still being explored.
The novel coronavirus on average infects 2.5 people, versus the flu’s 0.9 people.
“This particular strain of coronavirus, or SARS-CoV-2, is a novel virus, meaning that we haven’t ever seen this virus before. Most flu, cold-like other viruses we see that are very seasonal, are viruses that have actually morphed into another, different type of the same kind of virus, but our bodies already have a little bit of immunity built up to it,” CMU professor and co-lead of the Safe Together, Strong Together program Dr. Amy Bronson said. “Since this is a new virus, our bodies have not gone through the process of building antibodies, so we are not as easily able to defend ourselves.”
Myth: You can’t spread the coronavirus unless you’re showing symptoms.
You are actually able to transmit the coronavirus up to five days before showing any normal symptoms.
“Viruses are actually very smart. It’s really important to think about the fact that it needs a healthy host to transmit to in order to keep the virus alive,” Dr. Bronson said. “The virus is able to spread in what we call the incubation or early prodrome stage, two days prior to symptom onset or non-specific symptoms.”
Many infectious diseases feature a prodrome period, and coronaviruses can have one from three to five days in advance.
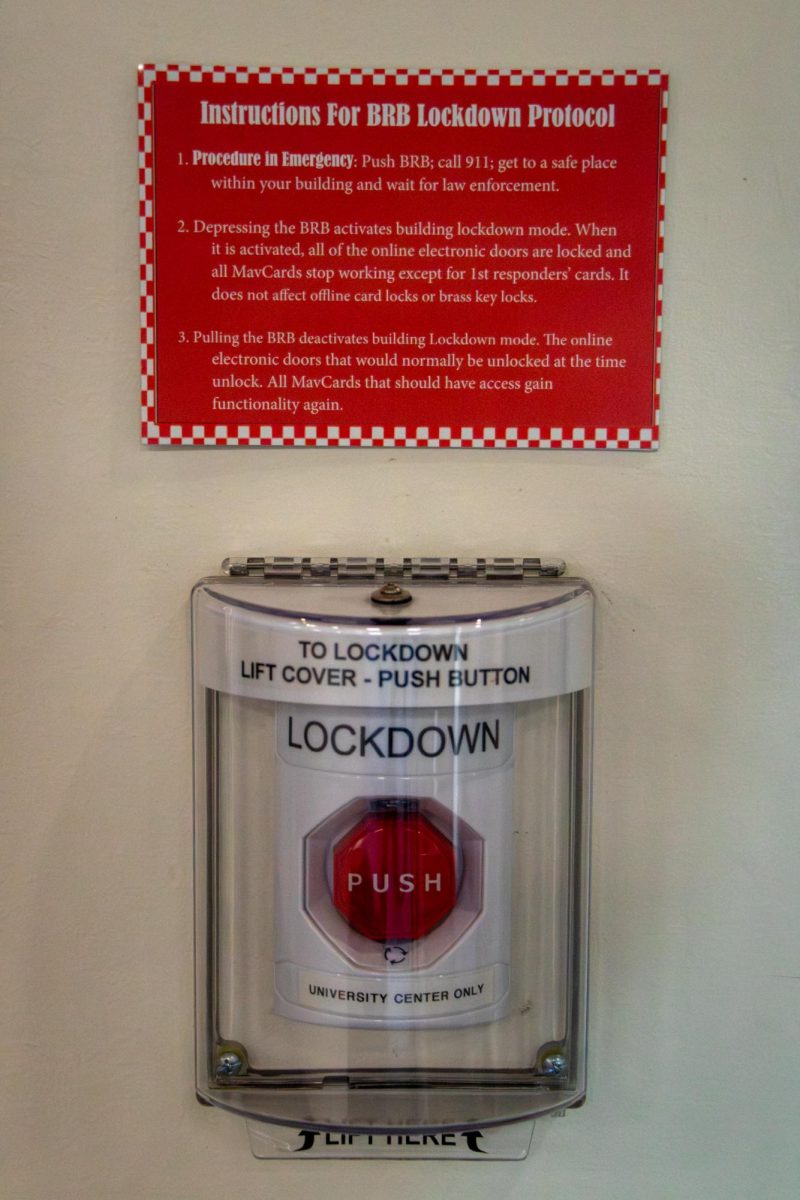
CMU has plans to help students who are exhibiting symptoms.
“The reality for us is that we’ve got to have multiple types of isolation and quarantine. You can kind of envision a variety of scenarios that we’re going to experience,” CMU Vice President and co-leader of Safe Together, Strong Together John Marshall said. “One is, you’re going to have sick students, like we do every year, where the flu and colds and everything [happens].
Marshall said the university will be careful about if students are starting to experience possible COVID-19 symptoms.
“We’re going to want to get that student on a consult with the student wellness center immediately, and then being able to see a practitioner as soon as possible and likely testing, based on what the practitioner determines,” Marshall said.
The university will also be doing randomized surveillance testing through campus all semester long, looking for prevalence of the virus and trying to identify and isolate it.
Myth: Hydroxychloroquine can cure coronavirus.
Hydroxychloroquine is an immunosuppressive drug approved by the United States Food and Drug Administration that primarily treats or prevents malaria, as well as rheumatoid arthritis and lupus.
Earlier in the year, hydroxychloroquine was possibly found to be beneficial toward treating coronavirus, and has been hailed a cure or treatment by some people, including United States President Donald Trump.
However, a study published in the Annals of Internal Medicine on July 16, 2020, found that the drug was no more effective than a placebo in those who were not hospitalized.
The randomized, double-blind, placebo-controlled study featured participants who were symptomatic, non hospitalized adults either with confirmed COVID-19 or probable COVID-19 and recent high-risk exposure. The study concluded that hydroxychloroquine in no way substantially reduced symptom severity in patients with mild COVID-19, and can be read here.
“When we have a virus that’s new or novel, we have some ideas of potential medications that have treated this type or this family of viruses before, but everything that we’re doing right now for treatment strategies are all piloting, meaning we don’t have a lot of longitudinal, or long-term data to help us determine if these have been effective agents for treating the symptoms that a person is having,” Dr. Bronson said.
Myth: COVID-19 is strictly a respiratory virus.
A respiratory virus affects the lungs, and COVID-19 has been thought to affect the lungs primarily through causing pneumonia. However, it increasingly looks like the virus can also affect the endothelial cells that line the body’s blood vessels, which protect the cardiovascular system.
A study published back in the medical journal The Lancet as early as April 2020 suggested possible heart complications from coronavirus. This could lead to blood clots and further heart problems. Effects are still being researched, and so far COVID-19 cannot be put definitively into one category.
Myth: Once you’ve caught coronavirus, you’re now immune and don’t need to worry about reinfection.
According to the Center for Disease Control’s website (CDC), “In some persons, after testing negative by RT-PCR in two consecutive samples, later samples can test positive again.”
This does not necessarily mean that the patient recovered and later caught the virus – the CDC says that a patient can be clinically recovered for weeks, but viral RNA can still be detected in respiratory samples from said patient.
In a study published in the New England Journal of Medicine on July 21, 2020, the journal reported “Our findings raise concern that humoral immunity against SARS-CoV-2 may not be long lasting in persons with mild illness, who compose the majority of persons with Covid-19.”
Their study found that antibodies in participants had a half-life of 73 days, and said of their findings: “It is difficult to extrapolate beyond our observation period of approximately 90 days because it is likely that the decay will decelerate.”
According to an article by The New York Times, a drop in antibodies after a few months is fairly normal, and it’s unlikely that one can get coronavirus more than once. The article goes on to talk about different ways that the body can fight a pathogen besides antibodies, such as memory T cells.
An absolute statement cannot be made on if one is immune from COVID-19 after infection, and studies on antibodies and other forms of bodily protection are ongoing. The one thing that can be absolutely said about COVID-19 is that we don’t know everything about it. As more studies and research comes out about the virus, we move one step closer to understanding how to deal with this global pandemic.







Michael Humbert • Aug 20, 2020 at 8:27 am
The Lancet study was retracted and yet you are still pushing it as factual. You are liars.
Almost everything you have written here is disinfo and fear porn. You call this journalism? You should be mightily ashamed.